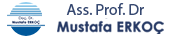
BPH, short for benign prostatic hyperplasia, is a common prostate condition in men. It is characterized by the enlargement of the prostate gland, a male organ located along the urinary tract. As a result, BPH can lead to urinary problems.
The normal growth of the prostate gland begins during adolescence and continues as men age. BPH occurs when the prostate gland grows excessively and exerts pressure, narrowing the urinary passages. This condition can make urination difficult and prevent the complete emptying of the bladder. In such cases, complications such as urinary tract infections, urinary retention, and others can develop.
BPH affects more than 50% of men and typically becomes noticeable after the age of 50, although it can occur earlier in some men. Common BPH symptoms include frequent urination, difficulty urinating, weak urine flow, a sense of incomplete bladder emptying, nocturia (waking up at night to urinate), and others.
What Are the Symptoms of BPH?
1. Frequent Urination: An increased need to urinate, including at night.
2. Difficulty Urinating: Effort may be required to initiate urination, and the urine stream can be weak or intermittent.
3. Weak Urine Flow: The flow of urine may become slow or may stop and start.
4. Incomplete Bladder Emptying: Feeling like the bladder is not completely emptied after urination.
5. Urinary Retention: Inability to fully empty the bladder, which can lead to discomfort and complications.
6. Urinary Tract Infections: BPH can increase the risk of urinary tract infections.
7. Blood in Urine: BPH may occasionally cause blood in the urine.
8. Urinary Incontinence: BPH can increase the risk of urinary incontinence
BPH symptoms typically develop gradually and can worsen over time. These symptoms can resemble those of other urinary tract conditions, so a medical examination may be necessary for an accurate diagnosis. If you experience BPH symptoms, your doctor can recommend appropriate treatment options.
How Is BPH Diagnosed and Treated?
The diagnosis of BPH (benign prostatic hyperplasia) involves various tests, including physical examination, blood tests, urine tests, prostate ultrasound, and urodynamic tests, in addition to evaluating your symptoms.
Treatment options may vary based on the severity of symptoms and the patient's age. For men with mild BPH symptoms, lifestyle modifications such as limiting fluid intake, reducing caffeine and alcohol consumption, and attempting to completely empty the bladder before leaving the restroom can help manage symptoms.
Medications can be used to reduce BPH symptoms. These medications may slow prostate growth or improve urinary flow. It's important to note that these medications can have side effects such as dizziness, low blood pressure, and sexual dysfunction, so it's essential to consult with your doctor to determine the most suitable medication for you.
Surgical intervention may be considered to alleviate or eliminate severe symptoms. Surgical treatment options may involve the partial or complete removal of the prostate. Surgery is typically preferred when other treatments are ineffective or when symptoms are severe.
The choice of surgical technique depends on factors like prostate size, patient age, and overall health. Your doctor will recommend the most suitable treatment options after assessing your symptoms and health condition.
Surgical Techniques for BPH (Benign Prostatic Hyperplasia
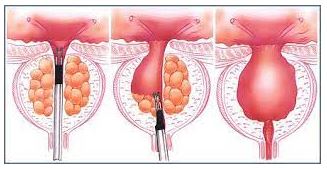
Surgery for BPH (benign prostatic hyperplasia) may involve the partial or complete removal of the prostate gland.
The most commonly used surgical methods for BPH surgery are as follows:
1. Transurethral Prostate Resection (TURP): In this method, an instrument is used to cut and remove excess tissue within the prostate gland. This procedure is performed through a small incision made with the assistance of an endoscope. TURP is the most common surgical approach used for BPH treatment.
2. Laser-Assisted Prostate Resection (LDP) (HOLEP-THULEP): These methods have become increasingly popular in recent years. Using laser technology, the entire prostate tissue is vaporized or removed in a few large pieces into the bladder. A morcellator (fragmentation device) is then employed to extract the pieces from the bladder. This technique is particularly suitable for treating larger prostates.
3. Transurethral Needle Ablation (TUNA): In this method, a needle is utilized to deliver heat to the prostate tissue, causing selected portions of the tissue to die off. TUNA aims to achieve symptom relief similar to TURP.
4. Transurethral Microwave Therapy (TUMT): TUMT involves the use of microwave energy to heat and shrink the prostate tissue. Similar to TURP, this method aims to alleviate symptoms effectively.
5. Open Surgical Removal of the Prostate: This method, often referred to as open surgery, is employed when dealing with large prostate glands that cannot be effectively treated using TURP or other endoscopic methods.
The choice of surgical technique depends on factors such as the size of the prostate, the age of the patient, and their overall health. Surgical intervention is typically considered when severe symptoms are present or when other treatments have proven ineffective